Trimethylamine-N-oxide (TMAO) might not be a household name, but it’s gaining attention in the world of health and wellness. This compound, produced by gut bacteria when we digest certain foods, is emerging as a key factor in the development of chronic diseases, particularly heart disease and non-alcoholic fatty liver disease (now called “metabolic dysfunction-associated fatty liver disease” or MAFLD). Understanding how TMAO contributes to this condition could help you take proactive steps to protect your liver and overall health.
What is a Fatty Liver?
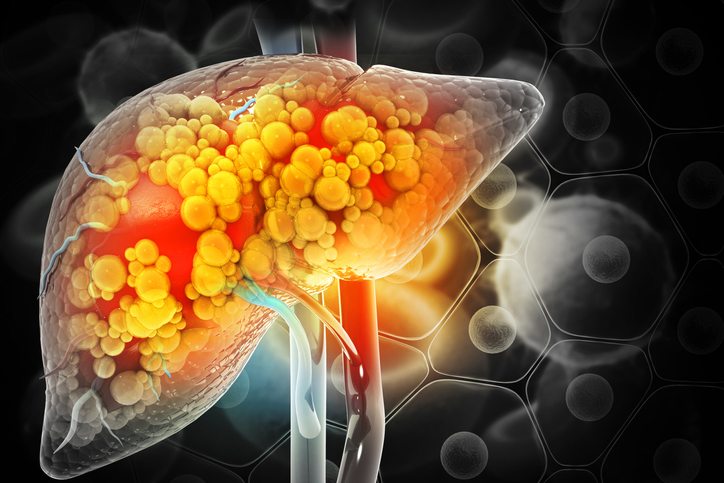
The term Non-Alcoholic Fatty Liver Disease (NAFLD) was an umbrella term for a spectrum of chronic liver conditions, characterized by excessive accumulation of fat in the cells of the liver. The term non-alcoholic was used because this type of liver disease is occurring in people who do not consume alcohol, such as children. Yet, in many respects, the nature and consequences of NAFLD are similar to what is seen in liver diseases of alcoholics who consume excessive amounts of alcohol.
NAFLD is very common and is often linked with type 2 diabetes and heart disease. Because NAFLD is closely tied to overall metabolic issues, experts are now using a new name: Metabolic-Associated Fatty Liver Disease (MAFLD). This updated term helps highlight the strong connections between fatty liver disease, diabetes, and heart disease, encouraging healthcare providers to check for these conditions together.
Since there are usually no overt symptoms of MAFLD it often goes undiagnosed, progressing into more a more serious liver condition known as non-alcoholic steatohepatitis (NASH). In NASH, increasing fat accumulation causes severe inflammation that damages the liver cells. This can lead to cirrhosis (severe scarring that impairs liver function as liver cells are repeatedly injured and die off), liver cancer, and liver failure (Magee et al., 2016).
Causes and Concerns
Known risk factors for MAFLD include obesity, diabetes, and metabolic syndrome. Research shows that 96 percent of significantly obese people have MAFLD, and it affects men at twice the rate as women (Teng et al., 2023). The most prominent underlying cause of all these conditions, including fatty liver, is the Standard American Diet (SAD), rife with sugary beverages, refined carbohydrates, excess animal protein and animal fats, low fiber, and low fruit and vegetable consumption.
High consumption of refined carbohydrates results in the carbs being converted to fat and stored in the liver, especially in people who are overweight or insulin-resistant (Sevastianova et al., 2012). The biggest culprit is excess consumption of beverages like soda and energy drinks that are sweetened with large amounts of sugar and high fructose corn syrup. Fructose is metabolized in the liver the same as alcohol and has been shown to be the main driver of liver fat accumulation in children and adults (Schwarz et al., 2015).
The best way to manage MAFLD is through lifestyle changes, like cutting back on sugary foods, but a new treatment targeting gut bacteria is also showing great promise.
What Is TMAO and How Does it Affect Fatty Liver Disease?
Trimethylamine-N-oxide (TMAO) is produced in the liver after gut bacteria break down certain nutrients, specifically L-carnitine, choline, and betaine, which are found in foods like red meat, eggs, and some fish. Research has already shown that high levels of TMAO may be linked to heart disease—but now it’s also being implicated in fatty liver disease.
Recent studies suggest that TMAO might play a role in worsening MAFLD by promoting liver inflammation and fibrosis, the scarring that can lead to cirrhosis.
One study found that mice fed a diet high in TMAO developed more severe fatty liver compared to those with lower TMAO levels. The mechanism behind this involves TMAO’s ability to disrupt fat metabolism and increase oxidative stress in the liver, which can accelerate the progression of MAFLD (Theofilis et al., 2022).
Can TMAO Levels Be Managed?
The good news is that you can manage your TMAO levels through diet and lifestyle choices. Reducing your intake of foods rich in L-carnitine and choline, such as red meat and eggs, can help lower TMAO production in your body. Instead, focus on a diet rich in plant-based foods, which do not contribute to TMAO formation and have been shown to support liver health.
Regular exercise is another key factor. Physical activity helps regulate your gut microbiome, which can lower TMAO production and improve liver health. Some studies also suggest that probiotics might help reduce TMAO levels, though more research is needed in this area.
Testing for TMAO Levels
If you’re concerned about your liver health and want to know more about your TMAO levels, it’s worth discussing with your healthcare provider. A simple blood test can measure your TMAO levels and help you understand your risk for fatty liver disease and other related conditions.
To summarize, TMAO might be a lesser-known player in the world of health, but its potential impact on fatty liver disease is something worth paying attention to. By understanding how your diet and lifestyle influence TMAO levels, you can take steps to protect your liver and overall health.
References:
Li, X., Hong, J., Wang, Y., Pei, M., Wang, L., & Gong, Z. (2021). Trimethylamine-N-Oxide pathway: A potential target for the treatment of MAFLD. Frontiers in Molecular Biosciences, 8. https://doi.org/10.3389/fmolb.2021.733507
Magee, N., Zou, A., & Zhang, Y. (2016). Pathogenesis of nonalcoholic steatohepatitis: Interactions between liver parenchymal and nonparenchymal cells. BioMed Research International, 2016, 1–11. https://onlinelibrary.wiley.com/doi/10.1155/2016/5170402
Schwarz, J., Noworolski, S. M., Wen, M. J., Dyachenko, A., Prior, J. L., Weinberg, M. E., Herraiz, L. A., Tai, V. W., Bergeron, N., Bersot, T. P., Rao, M. N., Schambelan, M., & Mulligan, K. (2015). Effect of a high-fructose weight-maintaining diet on lipogenesis and liver fat. The Journal of Clinical Endocrinology & Metabolism, 100(6), 2434–2442. https://doi.org/10.1210/jc.2014-3678
Sevastianova, K., Santos, A., Kotronen, A., Hakkarainen, A., Makkonen, J., Silander, K., Peltonen, M., Romeo, S., Lundbom, J., Lundbom, N., Olkkonen, V. M., Gylling, H., Fielding, B. A., Rissanen, A., & Yki-Järvinen, H. (2012). Effect of short-term carbohydrate overfeeding and long-term weight loss on liver fat in overweight humans. American Journal of Clinical Nutrition, 96(4), 727–734. https://doi.org/10.3945/ajcn.112.038695
Teng, M. L., Ng, C. H., Huang, D. Q., Chan, K. E., Tan, D. J., Lim, W. H., Yang, J. D., Tan, E., & Muthiah, M. D. (2023). Global incidence and prevalence of nonalcoholic fatty liver disease. Clinical and Molecular Hepatology, 29(Suppl), S32–S42. https://doi.org/10.3350/cmh.2022.0365
Theofilis, P., Vordoni, A., & Kalaitzidis, R. G. (2022). Trimethylamine N-Oxide Levels in non-alcoholic fatty liver disease: A systematic review and meta-analysis. Metabolites, 12(12), 1243. https://doi.org/10.3390/metabo12121243